Welcome to the the BVNS Neurotransmitter, written by Joli Jarboe, DVM, DACVIM (Neurology) – BVNS Leesburg
History:
Gizmo, a 3-year-old, M/N, 4.3 kg, Chihuahua-Jack Russell Terrier mix, was let outside on 2/16/21 and returned dragging his pelvic limbs. He was evaluated by primary care veterinarian the following day and placed on 5 mg Prednisone orally every 12 hours (tapering schedule) twice a day and 50 mg Gabapentin orally every 8 hours.
He was relinquished to the Animal Welfare League of Alexandria on 2/20/21 and referred to BVNS Springfield on 2/22/21. His neurological exam consisted of the following: normal cranial nerves; normal thoracic limb spinal reflexes; normal thoracic limb proprioception and placing responses; intact cutaneous trunci reflex; upper motor neuron pelvic limb spinal reflexes with absent proprioception and placing responses; intact superficial pain perception in all limbs and tail; perineal reflex present; thoracolumbar kyphosis; unable to stand in the pelvic limbs; severe paresis in the left pelvic limb with only weak hip flexion noted and plegic in the right pelvic limb; discomfort noted with palpation near the cranial lumbar spine with PS: ¼. Physical exam findings identified mild tartar, abnormal dentation, and bilateral grade I medially luxating patellas.
Neurologic Localization
T3-L3 and primary differential diagnoses being intervertebral disc related spinal cord injury, myelitis, neoplasia, other.
Advanced spine diagnostics (anesthesia, spine MRI, +/- spinal centesis and spinal fluid analysis) were recommended but declined in lieu of continued medical management while the rescue group considered Gizmo’s issues and diagnostics needed to know more. Tramadol, bladder management and exercise restrictions were added to his tapering Prednisone schedule and gabapentin.
Gizmo returned to BVNS Springfield on 3/2/21 for advanced spine diagnostics outlined on 2/22/21. At that evaluation, he was able to maintain a standing position in the pelvic limbs when placed in a standing posture by the examiner. He was able to take a few tentative steps in the pelvic limbs but demonstrated marked pelvic limb paraparesis and proprioceptive ataxia with intact spinal reflexes, intact superficial pain perception, and absent proprioception and placing responses. He had a strong voluntary tail wag. His thoracolumbar kyphosis and cranial lumbar discomfort (PS: ¼) persisted.
 |
 |
Diagnostics:
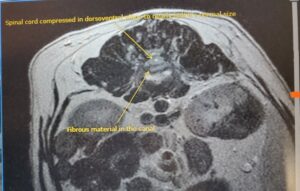
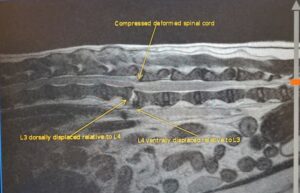
MRI performed on 3/2/21 identified a traumatic ventral subluxation of L3 relative to L2 causing moderate canal stenosis, moderate external cord compression, intrinsic (internal) cord injury processes, and regional inflammatory myositis. Fractures were also noted on the right 10th and 13th ribs. Left renal infarcts were also identified.
Diagnosis:
- Traumatic ventral subluxation of L3 relative to L2 causing moderate canal stenosis, moderate external cord compression, intrinsic cord injury processes, and regional inflammatory myositis
- Traumatic right 10 and 13 rib fractures
- Left sided, chronic, renal infarcts
Prognosis:
Fair to good with spine stabilization given presence of superficial pain perception and improving voluntary motor movement in the pelvic limbs.
Treatment:
Surgical Stabilization Performed at BVNS Leesburg with Dr. Jarboe on 3/4/21:
2.0 SOP stabilization with 2.0 self-tapping 14 mm screws (plate spanning caudal L1 to cranial L4. The plate did not have to be conformed as it was well seated along the accessory processes and concave aspect of the transverse processes. Encountered a large callous at the L2-L3 junction indicating a more chronic fracture than the initially presumed 2-week-old trauma relayed by the previous owners.
He was discharged the following day on a broad-spectrum antibiotic (cefpodoxime 50 mg orally once a day), muscle relaxant (diazepam 2 mg orally every 8 hours), analgesic (gabapentin 50 mg orally every 8 hours), analgesic (Tramadol 25 mg orally every 8 hours). Physiotherapy, bladder management, and exercise restrictions were continued.
Outcome: The following day, he was showing improved mobility in his pelvic limbs and improved comfort. At his 2 week post op recheck, he was walking in the pelvic limbs with mild paraparesis and proprioceptive ataxia. By four weeks post op, he was walking normally. His 8-week post op radiographs show continued alignment of the SOP construct. Best of all, he found his forever home with the BVNS Neurologist who first evaluated him late February 2022, Dr. Barker, and her wife Carolina. And they lived happily ever after!
Take home points:
- Sedated radiographs can help identify fractures, bone infections, and some bone and soft tissue cancers.
- Spine subluxations and fractures often carry a good prognosis with spine stabilization providing intact pain perception (nociception) and some degree of voluntary motor movement exists.
- Bladder management is a key component of caring for a non-ambulatory dog. Proper bladder management helps reduce detrusor muscle injury resulting in atony as well as helps reduce urinary tract infections. Muscle relaxants may help with owner assisted bladder care as muscle relaxants help reduced increased urethral sphincter tone allowing relaxation and easier emptying of the bladder with manual pressure.
- When addressing general inflammation suspected with spine trauma including intervertebral disc issues, consider reaching for a non-steroidal anti-inflammatory medication or, if using corticosteroids, consider using anti inflammatory doses (0.25 -0.5 mg/kg Prednisone PO BID tapering) rather than immunosuppressant doses (1-2 mg/kg Prednisone PO BID tapering).
- If a spine fracture is minimally displaced and pain perception is present in the pet’s limbs and owner has cost constraints , medical management could be considered with strict exercise restrictions for 8 weeks, physiotherapy, bladder management, analgesia, muscle relaxants, and NSAID or anti inflammatory corticosteroid.
Click HERE for a PDF version.
-->